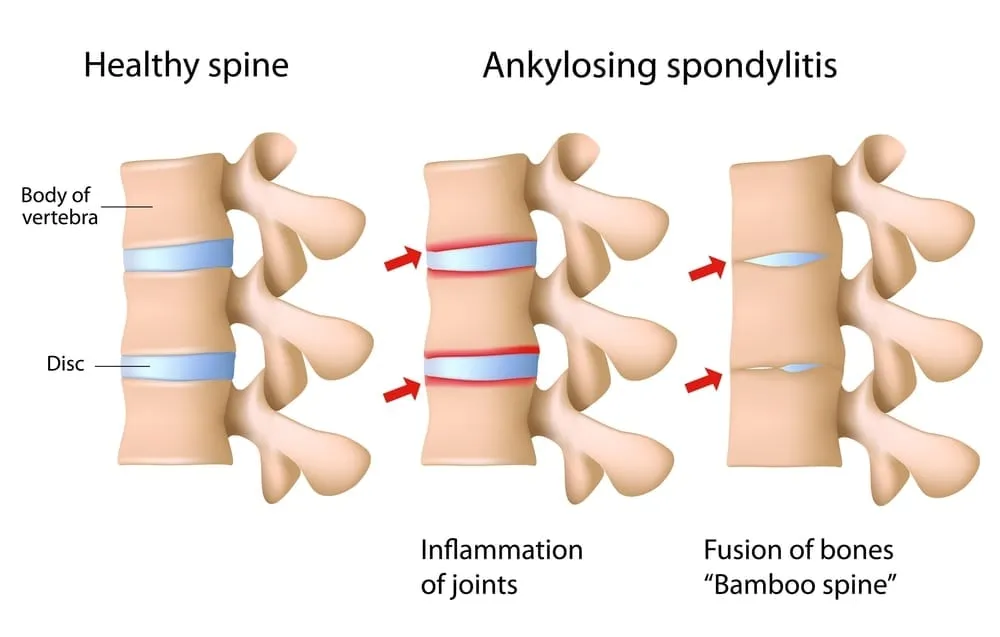
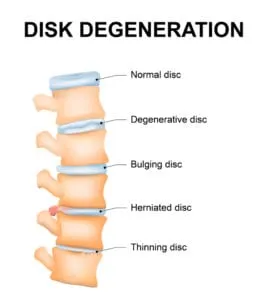
Ankylosing Spondylitis (AS) is a progressive disease that causes spinal vertebrae to slowly begin fusing together – especially those in the lower back near the base of the spine. The inflammation that affects the joints can also gradually affect other areas of the body, such as the hip and shoulder joints, the eyes, or the bowels. Symptoms are usually relatively minor in the earliest stages of the disease and may only present as decreased flexibility or a slightly ‘hunched’ posture. However, a progression of ankylosing spondylitis can lead to an inability to lift the head to a forward-looking position.
Did you know…
that the average age of onset for ankylosing spondylitis is between 17 and 45? But older people and children are also susceptible to the disease. AS is found in people of all ages and backgrounds, but occurs more frequently among men than women. One of the greatest risks for AS is among individuals who test positive for the HLA-B27 gene, which is easily identified in a diagnostic blood test.
Frequently Asked Questions
Am I at risk for developing ankylosing spondylitis?
There are no known lifestyle risk factors for ankylosing spondylitis – only age, genetics and gender play a role in whether a person will develop the disease. However, you may want to see a rheumatologist about this condition if you have a history of frequent gastrointestinal infections or a family history of ankylosing spondylitis.
What types of treatments are available for ankylosing spondylitis?
There is currently no cure for ankylosing spondylitis, but anti-inflammatories, TNF-blockers, physical therapy, and sometimes surgery can help manage pain, reduce stiffness, and potentially delay the progression of spinal deformity.
Is there anything I can do to help facilitate treatment for ankylosing spondylitis?
If you are diagnosed with ankylosing spondylitis, avoid smoking, which can significantly complicate the disease.